Not all people with Gorlin syndrome have the same symptoms, not even with family members who share the condition.
Symptoms of Gorlin syndrome can affect nearly every part of the body including, skin, bones and internal organs. Many symptoms do not cause the person with Gorlin syndrome any problems. Others, like basal cell carcinoma must be monitored closely as they can have significant impact on health. Some symptoms are congenital (present from birth) and others develop over time.


Basal cell carcinomas on the face of a person with Gorlin syndrome.
CCs are a common symptom of the disease.
Also known as basal cell skin cancer, basal cell carcinomas (BCCs) is the most common feature of Gorlin syndrome. About 90% of people with Gorlin syndrome will have one or more BCCs by the age of 35.
BCCs happen when the cells in the bottom layer of the skin (the basal layer) become cancerous. Most basal cell cancers occur on skin that is regularly exposed to sunlight or other ultraviolet light radiation such as what is generated by tanning beds and certain types of lasers. In people with Gorlin syndrome, BCCs can develop in areas of the body that have not been exposed to much sunlight.
Basal cell carcinomas have raised borders that can appear glossy and shiny. BCCs can also be pink, red or skin-colored, and may have darker flecks in them and be dome-shaped, flat, bumpy or scaly. Some BCCs develop a small crater in the center, ooze or bleed easily and crust over.
Basal cell carcinoma is the most common form of skin cancer in the US. One in five Americans (without Gorlin syndrome) will develop a BCC. This type of BCC is called sporadic basal cell carcinoma.
Treatment for BCCs depends on the size, depth and location of the BCCs on the body, the patient’s age and health status. BCC treatment is typically managed by a dermatologist.
A basal cell carcinoma can be classified into subtypes. “Superficial” is the least invasive type of BCC. The other BCC types include nodular, sclerosing and morpheaform, which is the most aggressive. A biopsy and pathology report are the only definitive way to know the subtype.

For more advanced BCCs, surgery may be required.
Knowing the BCC subtype is important to determining treatment. Because a person with Gorlin syndrome is likely to undergo multiple treatments for BCCs over his or her lifetime, the treatment approach is necessarily different than that of the “typical” skin cancer patient who may only undergo one or two surgeries.
There are several different types of treatments for basal cell carcinomas. These include surgery, topical treatments and oral medications. Surgery for BCCs are typically “outpatient” done in the provider’s office with local anesthesia. The patient returns home that day.
Treatments for basal cell carcinomas include:
Mohs surgery removes a thin layer of the BCC tissue. This layer is analyzed for cancer cells while the patient waits. If there is presence of cancer cells, the Mohs surgeon removes another layer for analysis. Once a layer is free of cancer cells, the wound is closed and the surgery is complete. Learn more about Mohs surgery.
Excisional surgery is the removal of the entire BCC growth and some skin around it for a safety margin. The incision area is closed with stitches and the growth is sent to the lab for analysis.
Curettage and electrodesiccation, where the BCC growth is first removed with a special tool and then the area underneath is dessicated, or burned, with a fine needle used specifically for this purpose.

BCC surgery is usually an outpatient procedure.
Cryosurgery destroys the BCC growth by freezing it. Liquid nitrogen is applied directly to the BCC causing the growth to blister, scab over and eventually fall off.
Photodynamic therapy (PDT) destroys BCCs by zapping them with a strong blue light after a topical “activating” agent is applied. Sunlight must be avoided for at least 48 hours after the procedure. PDT is used for superficial (thin BCCs) as it not effective on large or raised (nodular) BCCs. Photodynamic therapy is safer for people with Gorlin syndrome as it does not contain radiation.
Laser surgery, while not yet approved by the FDA for the treatment of superficial BCCs, uses a strong beam of light (the laser) to destroy BCCs.
Topical medications (imiquimod or 5 flurouracil) are applied to the tumor site multiple times of day for up to six weeks, depending on the type of medication.
Oral medications sonidegib (Odomzo) and vismodegib (Erivedge) are used for advanced cases of BCCs, adults with multiple BCCs, and those that are metastatic (spread to other parts of the body). Both cause severe birth defects and women must take caution to avoid pregnancy while on these medications. They cannot be used in children due to the risk of impaired bone growth. Click here to learn more.

Odontogenic Keraticys grow in the jawbone and can cause tooth loss if not treated promptly.
Odontogenic Keraticys is a benign (non-cancerous) cyst or tumor that grows in the lower or upper jaw bones. The cysts are formed from the cells and tissue that help develop teeth.
Odontogenic Keraticys are often found during routine dental x-rays or when pain, swelling and drainage develop in the area. They may be associated with impacted baby teeth, and can cause problems with the new teeth coming in.
Odontogenic Keraticys can return and must be treated aggressively. If Odontogenic Keraticys are left untreated they continue to grow, pushing out permanent teeth and damaging the jaw bones. They can expand into the sinus cavity and cause discomfort in the cheek(s).
Odontogenic Keraticys are treated by oral and maxilla-facial surgeons or otolaryngologists (ear, nose and throat physicians). Treatment for OKCs is surgery to remove the cysts.
Palmoplantar pits (palmar planter) are small depressions or dots on the palms of the hands or soles of the feet. Most people with Gorlin syndrome have pits – some may have a few of them and others may have hundreds.
The pits look similar to large pores and can be more noticeable when the skin has absorbed water (like after a bath). The words palmar and plantar refer to the areas where they are found most often – on the palms of the hands and the bottoms of the feet.

Pits on the palms of the hands are a common symptom of Gorlin syndrome.
Generally, palmoplantar pits are painless and cause no problems. If the pits grow or change or become infected, consult a health care provider.
Also called sebaceous, keratin or epithelial, epidermal cysts are small hard lumps that live just under the skin. Usually slow growing, epidermal cysts can appear anywhere on the body and rarely cause pain or other symptoms unless they become infected or drain.
Some epidermal cysts of the skin require no treatment. Others may need to be surgically removed. Plastic surgeons, dermatologists, and general surgeons do this type of procedure. If the epidermal cysts become infected, medical treatment may be necessary.

An example of macrocephaly in a young child.
Many people with Gorlin syndrome have large skulls (macrocephaly) and prominent foreheads (frontoparietal bossing). Most people with macrocephaly and frontoparietal bossing will experience no negative health effects. Others may require surgical intervention to correct the development, formation and fusion of the bones of the skull.
Infants, toddlers, and young children should have their head size monitored by their pediatrician. The provider will monitor the sutures (spaces between the skull bones) for proper growth and development.

An scan showing a brain with a calcified falx cerebri.
The falx cerebri is a tough membrane that separates the right and left sides of the brain.
The falx cerebri becomes calcified when calcium salts build up and cause the membrane to harden. Calcified falx cerebri is seen in children and adults with Gorlin syndrome and is very common.
A health care provider can identify calcified falx cerebri in an x-ray or brain scan. A calcified falx cerebri has no symptoms and does not affect health.
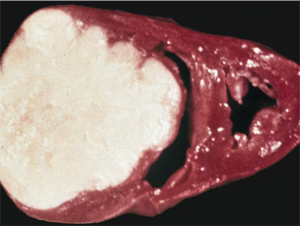
Ovarian fibromas are non-cancerous tumor-like growths on or near a woman’s ovaries. They are made up of an overgrowth of connective tissues. In women with Gorlin syndrome, ovarian fibromas most often appear on both of the ovaries at the same time.
Up to 30% of women with Gorlin syndrome are affected by ovarian fibromas. With proper monitoring and treatment, there is no evidence that suggests ovarian fibromas affect a woman’s fertility.
Ovarian fibromas usually do not cause any problems unless they are large.
Females with Gorlin syndrome should be monitored regularly for ovarian fibromas starting in their early teen years. Ovarian fibromas are detected using imaging such as MRI, CT scan or ultrasound of the lower abdomen.
If the ovarian fibroma is large and/or causing internal issues, surgical removal may be necessary.
A hamartoma is a benign (not cancerous) tumour-like growth in a bone. Hamartomas are made up of cells and tissues that grow abnormally.
Hamartomas generally do not cause problems. However, if a hamartoma develops in the foot, it is important to consult an orthopedic physician. Treatments may include casting and surgery.
A high-arched palate or high-vaulted palate is where the roof of the mouth is high and narrow. About 30% of U.S. children are born with a high-arched palate. Children with a high-arched palate may have trouble feeding as infants, difficulty breathing, sleep issues, speech problems and difficulty clearing nasal congestion.
People with a high-arched palate should be evaluated by a maxilla-facial surgeon or an otolaryngologist (ear, nose, and throat physician). Treatment for high-arched palate include the use of a tongue expander and exercises to reposition and strengthen the tongue. In more severe cases, surgery may be necessary.
Paranasal sinuses are the pockets or cavities of air in the bones of the skull around the nose and in the forehead. The role of the sinuses are many including helping to condition the air we breathe and increasing the sound of our speech.
Hyperpneumatization of the paranasal sinuses means that there is extra air-space in the sinuses around the nose. Generally, there are no symptoms or problems related to this symptom and no treatment is required.
Lumbarization of the sacrum is when the vertebrae of the sacrum (the large, triangle-shaped bone at the bottom of the spine) appear on x-ray like the lumbar (the spine in the abdominal area) vertebrae. The sacrum of an individual with lumbarization is not as fused as the normal sacrum.
Lumbarization of the sacrum is treated by an orthopedic surgeon or neurosurgeon. Treatments include non-steroidal, anti-inflammatory (NSAIDs) and pain medications and physical therapy. Surgery to correct the defect may be required if more conservative therapy does not help.

Kyphoscoliosis is when the spine turns both outward and to the side.
Kyphoscoliosis is a combination of kyphosis (when the spine turns outward) and scoliosis (when the spine curves into a “c” or “s” shape). In addition to disfigurement, kyphoscoliosis can cause pain, trouble breathing, stiffness fatigue and nerve issues.
People with kyphoscoliosis are treated by an orthopedic surgeon or a neurosurgeon if symptoms are bothersome. Treatments usually begins with physical therapy and back braces. In severe cases surgery may be necessary.
Narrow sloping shoulders are when the shoulders appear to be smaller than the hips and angle downward from the neck. Sloping shoulders generally do not have any symptoms but if they cause discomfort or limit motion, the person should be evaluated by an orthopedic surgeon.

Pectus excavatum causes the chest to appear sunken.
Pectus excavatum happens when the sternum (breastbone) and rib cage grow abnormally, causing sunken or caved in appearance of the chest.
Pectus carinatum happens when the breastbone and rib cage develop in a manner that causes the chest to jut out similar to a bird. Because of this, pectus carinatum is sometimes called “pigeon chest.”
Many people with pectus excavatum or carinatum experience no other symptoms related to these conditions. Sometimes these conditions can cause breathing problems, heart issues and pain in the chest and back.

Prognathism causes the lower jaw to stick out further than the upper jaw.
Prognathism is the position of the upper jaw in relation to the lower jaw. In mandibular (lower jaw) prognathism, the lower jaw protrudes or sticks out further from the upper jaw (maxilla). Prognathism of the maxilla means the upper jaw protrudes out further than the lower.
This problem can lead to misalignment of the upper and lower teeth. People with prognathism should be evaluated by their dentist, and possibly an orthodontist and oral surgeon.
People with Gorlin syndrome may have a variety of changes in the shape of their ribs. These include ribs that are splayed (turned outward), fused (stuck together), bifid (split in two at the end), and partially missing.

People with Gorlin syndrome may have abnormal shaped ribs.
Rib anomalies generally do not cause any symptoms and therefore do not require any treatment.
The metacarpal bone is the lower part of the ring finger (the fourth finger counting from the thumb). Some people with Gorlin syndrome have a shorter metacarpal bone than average. Generally, this change in the length of the bone does not cause any problems for the individual.
In spina bifida occulta, or closed spina bifida, one or more bones of the spine do not form correctly. People with Gorlin syndrome typically have spina bifida occulta in the bones of the neck (cervical vertebrae) or the upper/back (thoracic vertebra).
Unlike in spina bifida, the spinal column in spina bifida occulta is not significantly moved out of place. For this reason, spina bifida occulta usually does not cause any symptoms. Sometimes there are outward signs of spina bifida occulta such as a tuft of hair or a small dimple or birthmark on a child’s lower back.
In rare instances, the spinal cord may be compressed by abnormalities in the skeleton as a result of Gorlin syndrome. This may result in abnormal feet, numb or weak hands or feet, or problems with bladder and bowels.
People with spina bifida occulta of the cervical or thoracic vertebrae should be evaluated by a neurologist and or neurosurgeon who has experience with these spine abnormalities.
Often called a unibrow or monobrow, synophrys is a fusion of the two eyebrows above the bridge of the nose, creating a single eyebrow.
Some people with a unibrow choose to wax, shave or pluck the hairs in the middle to create the look of two eyebrows. Sometimes, the hair does not grow back after repeated removal.

Syndactyly results in fingers and/or toes that are fused together.
People with syndactyly have some or all of their fingers or toes fused together by tissue sometimes called “webbing.” Syndactyly is not typically painful but can affect the functioning of the hands or feet depending on the level of fusion.
Fingers and toes with syndactyly can be separated by a plastic surgeon or a hand surgeon.
Crossed eyes or strabismus is when of one or both eyes turn inward. Strabismus may happen to a person sometimes (intermittent) or be present all the time (constant).
Individuals with strabismus should see an ophthalmologist for treatment. Strabismus is first treated with a patch over the affected eye and or vision therapy. If those treatments do not work, surgery may be necessary.
Cardiac fibromas are benign tumors found in the heart of people with Gorlin syndrome.
Cardiac fibromas are benign (non-cancerous) tumors of the heart made up of connective tissues. These tumors usually occur in infants and children.
Symptoms of cardiac fibromas depend on the size and location of the tumor. Symptoms may include irregular heartbeat, heart murmurs, bluish skin, fainting and dizziness.
Cardiac fibromas may be diagnosed with an MRI or CT scan, sonogram and/or a tissue biopsy. Cardiac fibromas are treated with careful monitoring by a cardiologist and possible surgery by a cardiothoracic surgeon. Not all individuals with cardiac fibromas require immediate surgery. In very extreme cases, a heart transplant operation may be required.
Lymphomesenteric cysts are benign (non-cancerous) tumors of the abdomen that can cause belly pain, and bowel blockage when large or widespread. These cysts are made up mostly of the fluid from the lymph system.
If abdominal pain develops, seek care. The extent of the condition may be diagnosed by ultrasound, MRI or CT scan. Treatment for advanced or widespread lymphomesenteric cysts is surgery to remove the blockage.
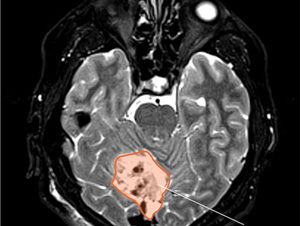
Medulloblastoma can develop in the first two years of life for children with Gorlin syndrome.
Medulloblastoma is a malignant (cancerous) brain tumor that grows quickly. It is seen most often in children younger than 8 years. In those with Gorlin syndrome, medulloblastoma may develop in the first two years. More boys with Gorlin syndrome develop this tumor than girls.
Symptoms of medulloblastoma include headache, vomiting, nausea, sleepiness, and difficulty with coordination. There could be changes in behavior, appetite, as well as unusual eye movements.
The diagnosis is made by CT scan or MRI of the brain. Once diagnosed, the child should be seen by a neurosurgeon and possibly an oncologist as soon as possible. Depending on the location of the medulloblastoma, survival rate for this cancer is up to 80%.
Treatment options for medulloblastoma include surgery, radiation and/or chemotherapy. When discussing treatment options, it is important to recognize that the use of radiation therapy may induce the growth of multiple basal cell carcinomas in patients with Gorlin syndrome. The risks and benefits of each treatment option should be carefully considered by the child’s entire care team.
Meningiomas are generally slow growing, benign (non-cancerous) brain tumors that come from the covering of the brain and spinal cord. They do not grow from the brain tissue itself.
Symptoms of meningiomas vary depending on the location of the tumor. Symptoms may include headache, weakness of an arm or leg. Less common signs include personality changes, seizures, and vision problems.
Meningioma is diagnosed by a CT scan or MRI of the brain and typically managed by a neurosurgeon.

Hypertelorism results in the appearance of wide-set eyes.
Ocular hypertelorism is a wide distance between the eye sockets, resulting in “wide-set” appearing eyes. Occasionally, hypertelorism can cause visual problems, but usually this is not the case. Severe cases of ocular hypertelorism are treated in childhood with surgery.